How to Reduce Swelling After Plastic Surgery

Picture this: you've just had the cosmetic procedure you've been planning for months (or years), and you're expecting to wake up looking like an Instagram filter brought to life. Instead, you catch a glimpse of yourself in the mirror and wonder if someone accidentally inflated you overnight. Welcome to the wonderful world of post-surgical swelling – where even the most stunning surgical results are temporarily hidden behind puffiness that makes you question every decision that led to this moment.
Before you start spiraling into a panic about whether you've made a terrible mistake, take a deep breath. That puffy, inflated appearance staring back at you isn't your final result – it's actually a completely normal and temporary part of the healing process. Every single person who has ever undergone plastic surgery has been exactly where you are right now, wondering when their normal appearance will return. You're not alone in this journey, and what you're experiencing is as predictable as it is temporary.
The good news? You're not powerless in this process. There are specific, science-backed strategies you can use to help your body reduce swelling more efficiently and reveal your beautiful new contours sooner. Think of your recovery as a partnership with your body that starts long before your surgical procedure even begins. Every choice you make can either help or hinder your body's natural deflation process.
This article will walk you through everything you need to know about conquering post-surgical swelling. We'll cover the immediate post-op survival tactics, the medium-term recovery strategies, and the long-term lifestyle choices that can dramatically impact how quickly you see your final results. By the time you're done reading, you'll have a complete action plan for working with your body's healing process rather than against it.
Understanding Post-Surgical Swelling: The Basics
Think of your body's response to surgery like an overly protective security system that doesn't distinguish between a break-in and routine maintenance. When your surgeon makes incisions and rearranges tissues, your immune system floods the area with protective fluids and inflammatory cells, creating the characteristic puffiness that peaks within 2-3 days and gradually improves over weeks and months.
Here's what nobody tells you: the extent of your swelling isn't necessarily related to how well your surgery went. Key factors that influence swelling include procedure type, location, and your individual healing response. More extensive procedures and areas with loose skin typically swell more dramatically – it's completely normal and expected, not a sign that something's wrong.
Normal swelling should be symmetrical, gradually improve over time, and not be accompanied by increasing pain or fever. While it's understandably concerning to see significant changes in your appearance, remember that this is your body working exactly as it should to protect and heal your surgical sites. Contact your surgeon immediately if swelling suddenly worsens, becomes asymmetrical, or is accompanied by concerning symptoms.

SHOP BEFORE + AFTER VITALS FOR POST-SURGERY SWELLING
The First 72 Hours: Your Make-or-Break Window
These first three days are admittedly the most challenging part of your recovery journey. While you're dealing with discomfort and the shock of seeing significant swelling, this critical window represents your golden opportunity to set the tone for your entire healing process. Think of these techniques as your recovery toolkit – each one working together to help your body calm down from surgery mode.
Cold therapy works like a gentle negotiation with your blood vessels, convincing them to contract and reduce fluid leakage. Use 15-20 minute cold applications with 20-minute breaks. Frozen peas work excellently for facial procedures because they conform to every contour; gel ice packs work well for body procedures. Always use a barrier between ice and skin – frostbite is definitely not part of your beauty plan.
Master Elevation Techniques
Think of elevation as working with gravity instead of against it. Keep surgical areas elevated above heart level whenever possible. Sleep in an elevated position for facial and upper body procedures – yes, it feels awkward at first, but your morning reflection will thank you. A back sleeping pillow designed for post-surgery recovery can make this transition much easier and will help boost both sleep and healing following surgery.
Start Anti-Inflammatory Nutrition Immediately
Here's what most people don't realize: your body is running a 24/7 repair operation right now, and it needs premium fuel to do its job efficiently. Begin taking specialized recovery supplements as soon as cleared by your surgeon, and heads up - they should actually be started before surgery. Bio-enhanced vitamin C formulations can reduce inflammation while supporting collagen synthesis without the digestive upset of standard vitamin C supplements. These specialized forms achieve significantly higher retention in your body when tissues need it most for healing.
Optimize Hydration Balance
Think of hydration like Goldilocks – not too little, not too much, but just right. Drink moderate amounts of water consistently. Avoid excessive fluid intake which can actually worsen swelling. Consider electrolyte balance over pure water volume.
Follow Positioning Guidelines Religiously
Your surgeon's positioning instructions aren't suggestions – they're prescriptions for optimal healing that can dramatically impact your swelling levels. Avoid sleeping flat or on your stomach for almost all cosmetic procedures, but be sure to check with your surgeon in advance. Proper positioning during these critical first days can make the difference between manageable swelling and prolonged puffiness.
Weeks 1-2: The Active Healing Phase
Once you've survived those initial challenging days, you enter what many patients describe as the most psychologically demanding phase of recovery. Your body is working around the clock to repair and rebuild, and while the peak swelling may have passed, you're still dealing with significant changes that require patience and active management. Remember, this is completely normal – you're not healing "wrong" if progress feels slower than expected.
Implement Gentle Movement
Protocol Think of movement like priming a pump – you need just enough action to get your lymphatic system flowing again. Start 5-10 minute walks every few hours to activate lymphatic drainage. Your lymphatic system is like your body's cleanup crew, and gentle movement helps them do their job more efficiently. Gradually increase duration as tolerated, but stop if swelling increases significantly after activity – that's your body's way of saying "not yet."
Maximize Compression Garment Benefits
Consider your compression garments as your 24/7 support team, providing consistent, therapeutic pressure to minimize fluid accumulation. Wear them consistently for optimal fluid control. Ensure proper fit: snug support without numbness or tingling. If you feel like you're being squeezed by a boa constrictor, it's too tight. If it feels loose enough to slide around, it's not doing its job. Replace if sizing changes during recovery.
Optimize Protein Absorption for Tissue Repair
Here's something that surprises most people: your protein needs skyrocket during healing, but absorption becomes the real challenge for swelling reduction. When your body can't properly break down and utilize protein, damaged tissues remain inflamed longer as they lack the amino acid building blocks needed for repair. It's like trying to build a house with half the necessary materials.
Specialized formulations like Before + After Vitals include proteolytic enzyme complexes that can double amino acid absorption from dietary protein. Clinical trials show these advanced enzymes dramatically improve your body's ability to utilize protein for tissue repair and swelling reduction by ensuring damaged tissues get the nutrients they need to resolve inflammation and return to normal.
Consider Professional Lymphatic Drainage
Professional lymphatic drainage is like giving your body's drainage system a gentle tune-up. Schedule sessions with trained professionals familiar with post-surgical care. This specialized massage helps restore normal lymphatic flow disrupted by surgery – but only trust someone who understands the delicate nature of your healing tissues.
Support Gut Health for Better Healing
Here's what most people don't expect: surgery and medications can disrupt your digestive balance, creating a domino effect that impairs nutrient absorption and creates systemic inflammation throughout your body. When your gut microbiome is disrupted, it triggers inflammatory responses that interfere with your body's natural healing processes. Think of your gut as mission control for your immune system – when it's not functioning optimally, everything else struggles too. Advanced synbiotic complexes that combine targeted probiotics with prebiotics help maintain digestive health, reduce post-surgical bloating, and support immune regulation that directly impacts how quickly swelling resolves.
Focus Anti-Inflammatory Nutrition
Your food choices during this phase are like fuel for your healing engine. Emphasize leafy greens, fatty fish, and berries – these are nature's anti-inflammatory powerhouses. Avoid processed foods and excessive sodium that can worsen fluid retention and essentially work against all your other swelling-reduction efforts.
Weeks 3+: The Patience Testing Phase
As you move beyond the three-week mark, you enter what many patients find to be the most emotionally challenging part of recovery. The dramatic improvements of early healing start to plateau, and you're left dealing with subtle, persistent changes that test your patience more than the actual surgery did. This is completely normal – you're not imagining things, and your healing isn't stalled.
Introduce Self-Massage Techniques
Think of self-massage as having a gentle conversation with your tissues, encouraging stubborn fluid to finally take the hint and move along. Use gentle upward strokes toward your heart to encourage lingering fluid drainage. Apply light pressure and avoid direct pressure on surgical sites – you're coaxing, not forcing.
Add Heat Therapy (When Approved)
Once your surgeon gives the green light, gentle heat therapy can be like opening the doors for better circulation to flow through your tissues. Always get surgeon approval before introducing heat. Avoid saunas and hot tubs for several more weeks – your tissues aren't ready for that level of intensity yet.
Enhance Collagen Production for Tissue Strength
Here's where the long-term magic happens: supporting your body's ability to build stronger, more resilient tissue architecture. Support long-term healing with hydrolyzed collagen that stimulates your skin cells to produce more natural collagen. Strong, well-structured collagen networks help tissues return to their normal architecture more quickly, reducing the prolonged swelling that occurs when tissues remain loose and inflamed. Think of collagen as the scaffolding that helps everything settle into its proper place. Clinical studies show specialized collagen peptides can improve skin elasticity by up to 15% in just four weeks, creating stronger, more resilient tissue at surgical sites that resolves swelling faster and maintains results better over time.
Progress Activity Levels Strategically
Gradually increasing your activity is like slowly turning up the volume on your normal life. Start with low-impact exercises before progressing to more intense workouts. Your body will give you clear feedback about when you're ready for each step up – listen to those signals rather than pushing through discomfort.
Manage Hormonal Fluctuations
Here's something that catches many people off-guard: hormonal changes can cause temporary swelling flare-ups that have nothing to do with your surgical healing. Expect temporary swelling increases due to menstrual cycles, stress, or sleep disruption. Track patterns to distinguish normal fluctuations from potential complications – this knowledge can save you from unnecessary worry.
Maintain Realistic Timeline Expectations
This might be the hardest truth to accept: final results can take 6-12 months, and that's not your surgeon being overly conservative. Subtle swelling changes are normal during this extended healing period. What you see in the mirror at three weeks is not your final result – try to resist the urge to judge your outcome too early in the process.
Lifestyle Optimization: The Hidden Game-Changers
Here's where the real healing magic happens behind the scenes. While everyone focuses on ice packs and compression garments, these lifestyle factors often make the difference between average recovery and exceptional results. Think of these as your secret weapons for faster, more comfortable healing.
Upgrade Your Recovery Nutrition BEFORE Your Procedure
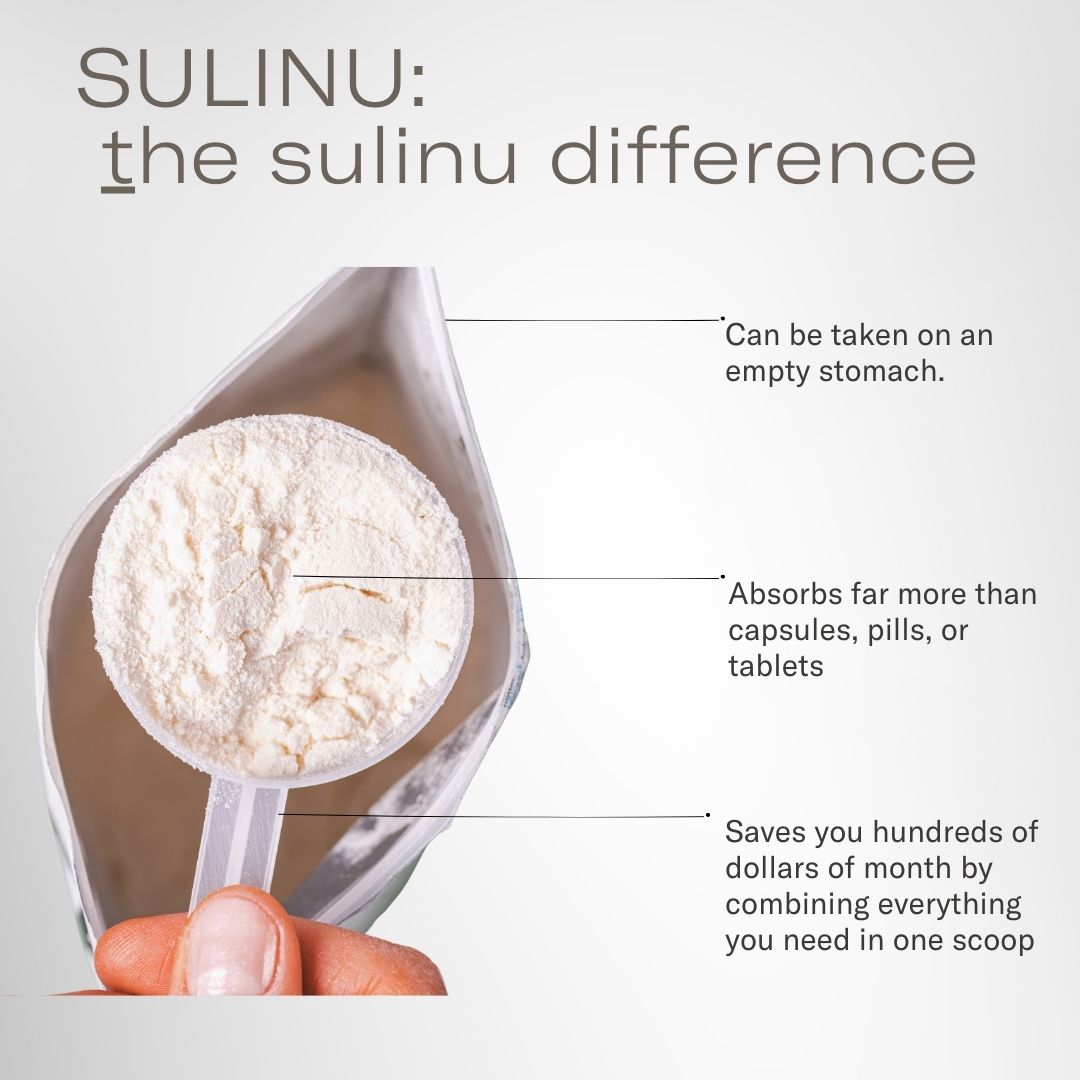
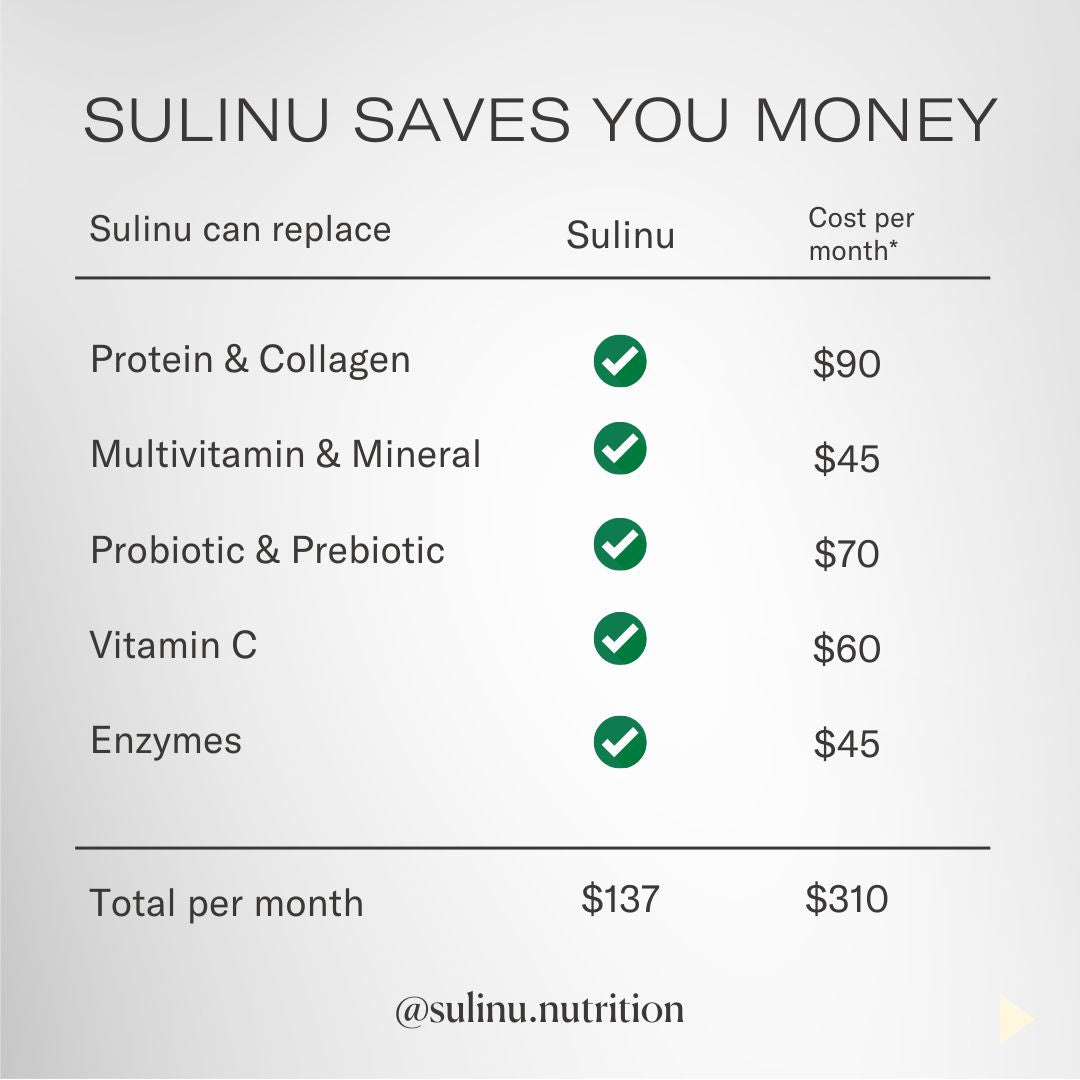
Here's what nobody tells you about supplements during recovery: standard multivitamins and basic supplements often fall short during the intense healing demands of surgical recovery. It's like trying to fuel a race car with regular gas. Comprehensive post-surgical formulations like Sulinu Before + After Vitals provide targeted nutrients in forms optimized for absorption when your body needs them most.
The key players that make the difference: Advanced vitamin C formulations achieve 233% higher retention compared to standard forms, ensuring optimal anti-inflammatory activity where swelling occurs while avoiding digestive upset. Proteolytic enzyme complexes can double amino acid absorption – the essential building blocks needed for tissue repair and swelling reduction. Specialized collagen peptides can improve skin elasticity by up to 15% in just four weeks, creating stronger, more resilient tissue at surgical sites.
Think of these specialized formulations as upgrading from basic tools to professional-grade equipment when your body needs peak performance most. For the best results, start your supplement protocol before your surgery date.
Target Anti-Inflammatory Foods
Your food choices are essentially medicine during recovery – every meal is an opportunity to either fuel healing or fuel inflammation. Prioritize omega-3 rich fatty fish, antioxidant-packed berries, leafy greens, and nuts. These foods work like nature's own anti-inflammatory pharmacy. Eliminate processed foods, refined sugars, and excessive sodium that trigger inflammatory responses and worsen fluid retention – they're essentially working against every other effort you're making to reduce swelling.
Optimize Digestive Health
Here's something that surprises most people: surgery and medications dramatically disrupt gut health, creating a ripple effect that impairs nutrient absorption and increases systemic inflammation throughout your recovery. A disrupted gut microbiome triggers inflammatory cascades that interfere with your body's natural anti-inflammatory processes, essentially working against your swelling reduction efforts. Think of your gut as the foundation of your healing – when it's compromised, everything else struggles too. Advanced synbiotic formulations that survive harsh stomach acids help maintain digestive balance, reduce inflammatory responses that contribute to persistent swelling, and support optimal nutrient absorption needed for tissue repair and inflammation resolution.
Master Stress and Sleep Management
Your emotional state and sleep quality have a more direct impact on swelling than most people realize. Chronic stress elevates cortisol, which essentially tells your body to stay in inflammatory mode – completely counterproductive to your healing goals. Poor sleep does the same thing, creating a cycle where inadequate rest leads to more inflammation and longer recovery times. Develop stress-reduction techniques within your physical limitations and prioritize sleep quality over quantity. Think of good sleep as your body's prime time for repair work – don't shortchange this critical healing window.
Warning Signs: When Normal Becomes Concerning
While most post-surgical swelling follows predictable patterns, contact your surgeon immediately if you experience:
-
Sudden worsening of swelling after initial improvement
-
Significant asymmetry in bilateral procedures
-
Swelling accompanied by fever, severe pain, or unusual discharge
-
Any concerning changes that feel fundamentally different from expected healing
Trust your instincts - experienced surgeons would rather evaluate false alarms than miss serious complications.
Your Most Pressing Questions Answered
"How long am I going to look like this? I need a realistic timeline."
Recovery timelines vary dramatically based on your specific procedure and individual healing characteristics. Most obvious swelling typically resolves within 4-6 weeks, but here's the reality check nobody prepares you for: subtle changes can continue for 6-12 months or even longer. Facial procedures often show faster initial improvement, while body contouring procedures may take longer to fully settle. Your surgeon can provide more specific timelines based on your particular procedure, but patience truly is part of the process.
"Why does my swelling seem to change every single day?"
This daily rollercoaster is absolutely normal and can be incredibly frustrating! Daily fluctuations in swelling are influenced by factors like activity level, sleep quality, sodium intake, hormonal changes, weather, and even stress levels. What matters is the overall downward trend over weeks and months, not day-to-day variations. Many patients notice they look better in the morning and more swollen by evening – this is your body's normal response to gravity and daily activities.
"Is there anything I can actually do to speed this up?"
While you can't force your body to heal faster than its natural pace (trust us, many have tried!), you can certainly create optimal conditions for healing. Think of it like tending a garden – you can't make plants grow faster, but you can provide the best soil, water, and nutrients. Proper nutrition, adequate rest, gentle movement as approved by your surgeon, consistent compression garment use, and avoiding inflammatory foods all work together to support your body's natural healing timeline.
"Everyone keeps telling me different things about heat versus ice. What's the real answer?"
The transition from ice to heat varies by procedure and surgeon preference, which explains all the conflicting advice you're hearing. Generally, ice is preferred for the first 48-72 hours to control initial inflammation. After this period, some surgeons recommend alternating heat and ice, while others prefer continued cold therapy for longer periods. Here's the golden rule: follow YOUR surgeon's specific instructions rather than well-meaning advice from friends or online forums. Never introduce heat therapy without specific approval from your surgical team.
"My compression garment feels different every day – is something wrong?"
This is completely normal and often catches people off guard. Compression garments feel different based on daily swelling fluctuations, how long you've been wearing it, and even factors like temperature and humidity. Some variation is expected, but if you experience severe discomfort, numbness, or circulation problems, the garment may need adjustment or you may need a different size. Think of it like a barometer for your healing progress.
"Could my medications be making the swelling worse?"
Yes, several medications can definitely affect swelling levels, and this often surprises patients. Blood pressure medications, hormones, some antidepressants, and NSAIDs can all influence fluid retention and inflammation. Always inform your surgeon about all medications and supplements you're taking – even things that seem unrelated. Never start or stop medications during recovery without approval from your healthcare team.
"At what point should I actually be worried about my swelling?"
While some swelling can persist for many months, contact your surgeon if swelling suddenly worsens after improving, becomes significantly asymmetrical, is accompanied by other concerning symptoms, or if you're simply worried about your healing pattern. Trust your instincts – if something feels fundamentally different from what you were prepared for, it's always appropriate to reach out. Your surgical team would rather evaluate ten false alarms than miss one serious issue.
"Is it normal to feel emotional about how I look during recovery?"
Completely normal, and this emotional aspect often catches patients off-guard! The psychological journey of recovery can be just as challenging as the physical healing. Seeing swelling when you're expecting beautiful results can be emotionally difficult. Remember that what you see in the mirror during early recovery is not your final result. Give yourself permission to feel frustrated while maintaining perspective about the healing timeline – you're not being dramatic, this process is genuinely challenging.
"How can I tell if this is normal healing versus something being wrong?"
Normal healing swelling gradually improves over time, is relatively symmetrical in bilateral procedures, and isn't accompanied by increasing pain, fever, or unusual discharge. Concerning swelling worsens over time, is significantly asymmetrical, or occurs alongside other worrisome symptoms like fever or severe pain. When in doubt, contact your surgical team for evaluation – that's what they're there for, and experienced surgeons would rather address your concerns than have you worry unnecessarily.
"Can I travel while I still have significant swelling?"
Travel restrictions depend on your procedure, healing progress, and travel plans. Air travel can worsen swelling due to cabin pressure and prolonged sitting, so many surgeons recommend waiting at least 1-2 weeks before flying. If you must travel, compression garments become even more important, and you'll need to move around frequently. Always get clearance from your surgeon first – they know your specific situation best.
Important Medical Disclaimer
This content is provided for educational and informational purposes only and should never be considered a substitute for professional medical advice, diagnosis, or treatment. Every person's surgical experience and healing process is unique, influenced by factors including the specific procedure performed, individual health status, age, genetics, and adherence to post-operative care instructions.
If you experience any concerning symptoms during your recovery period – including excessive or worsening swelling, signs of infection, severe pain, or any of the warning signs discussed in this article – contact your surgeon immediately or seek appropriate emergency medical care. Do not delay seeking professional medical evaluation based on information found in this or any other online resource.
The mention of specific products, supplements, treatments, or techniques in this article does not constitute medical advice or professional endorsement. Always consult with your healthcare providers before starting any new supplements, treatments, or significant changes to your recovery routine, as these may interact with prescribed medications or interfere with your healing process.
Before + After Vitals



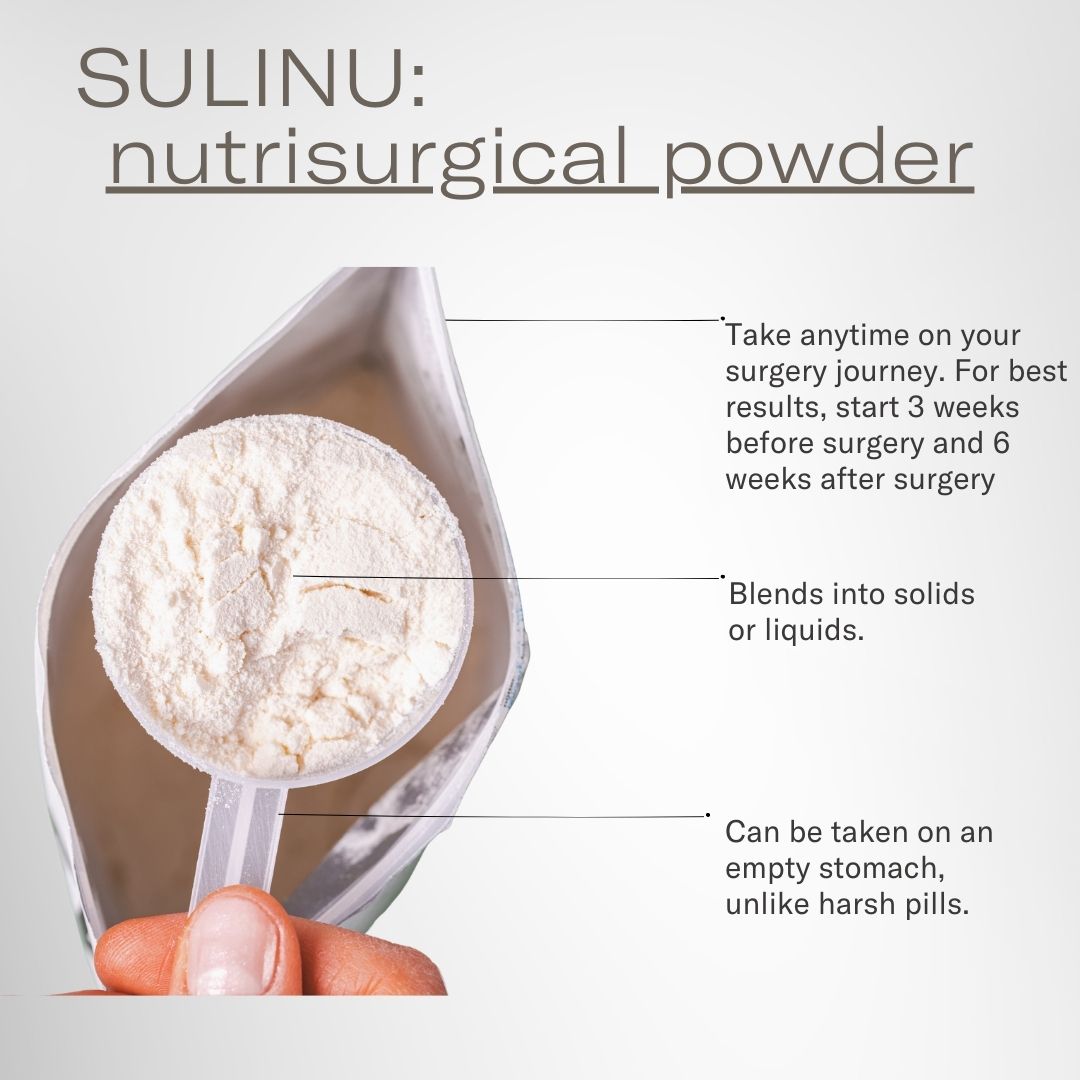






NUTRISURGICAL VITAMIN POWDER -(bag: Vanilla)
**FREE SHIPPING for orders over $150!!**
- 100% Money Back Guarantee
- Discreet Shipping-Your privacy is important
- We recommend 3 bags for any surgery for the best results
This Complete Surgery Powder gives you EVERYTHING you need IN ONE SCOOP.
Pre and Post Surgery Supplements for that near-invisible scar look.
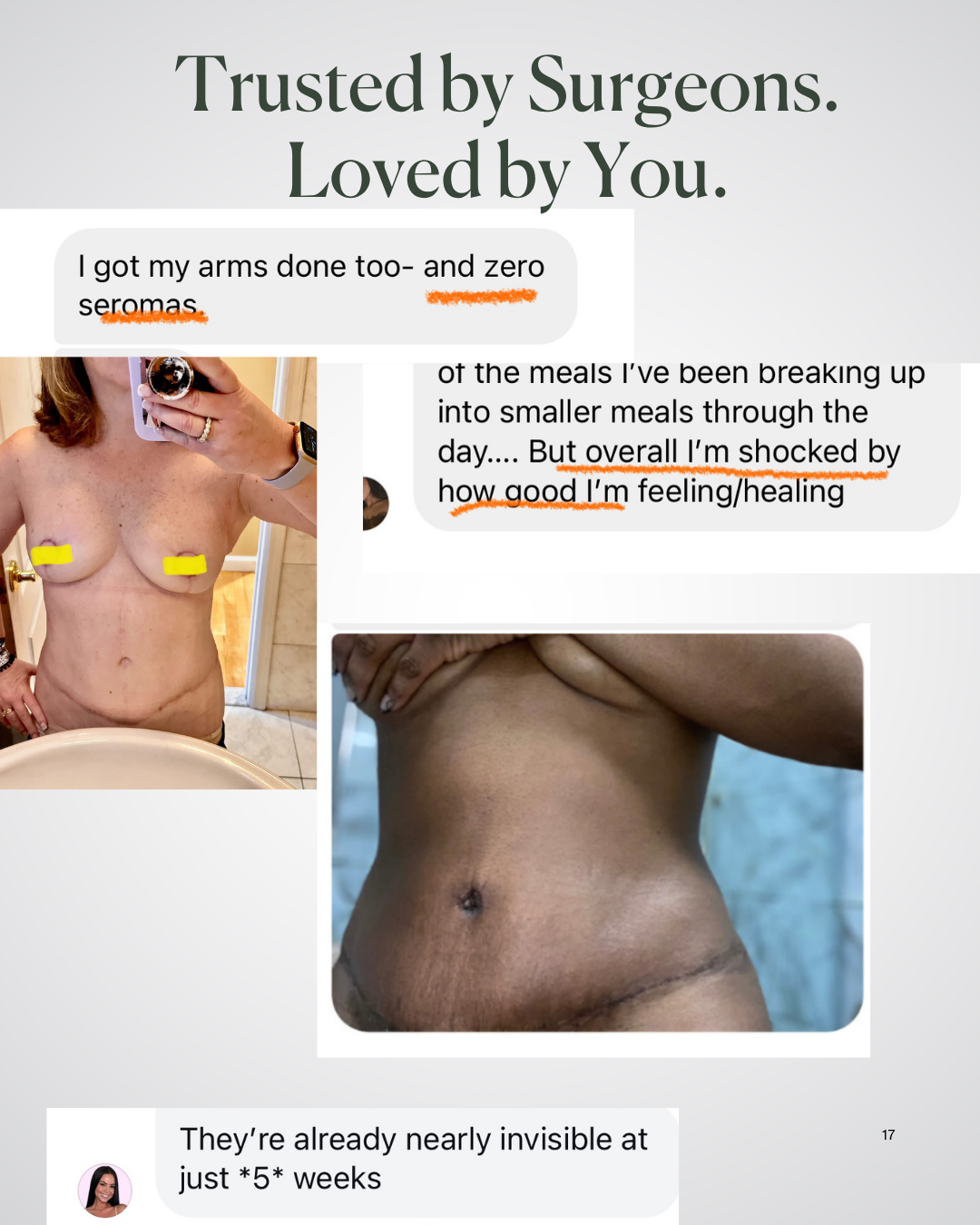
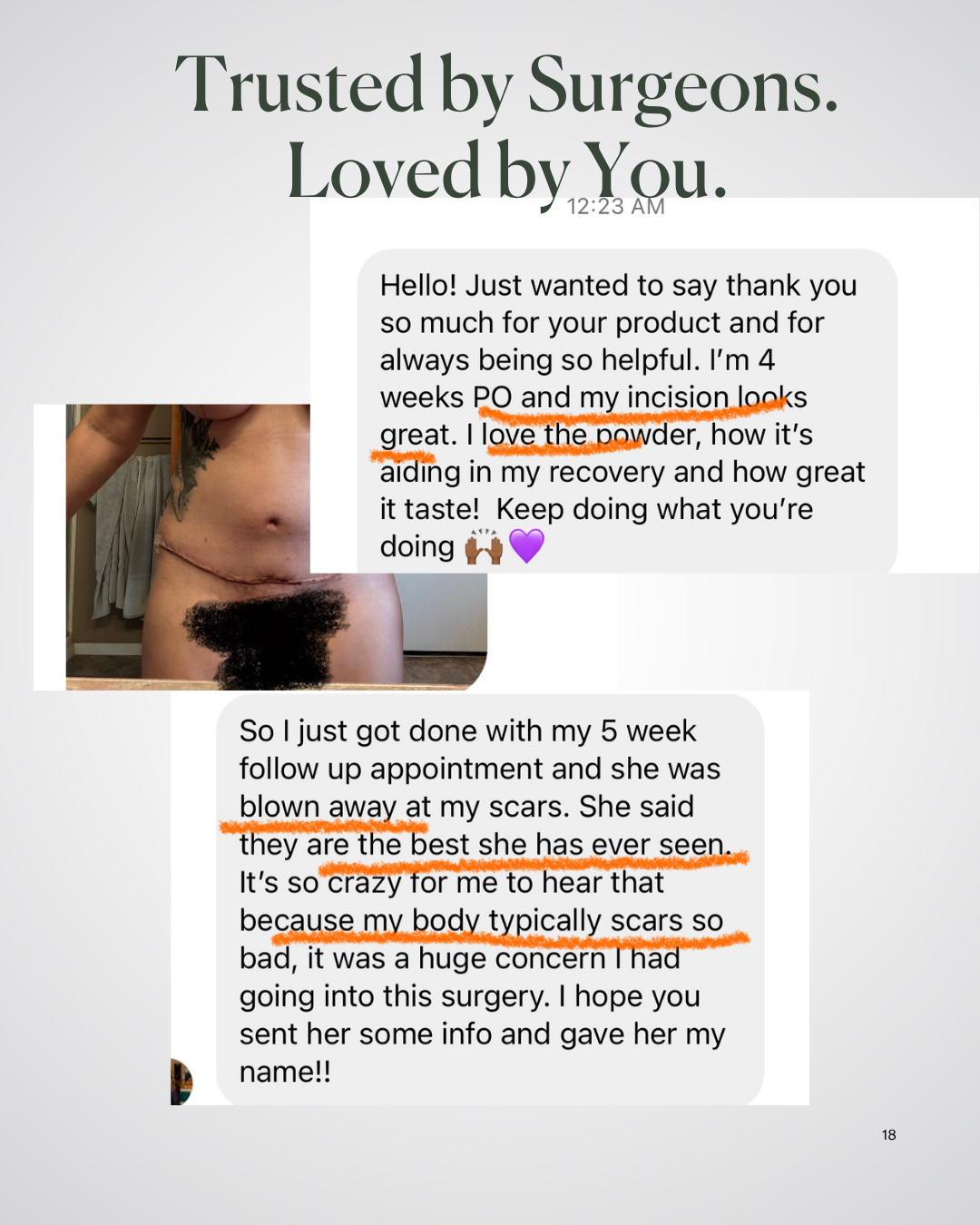
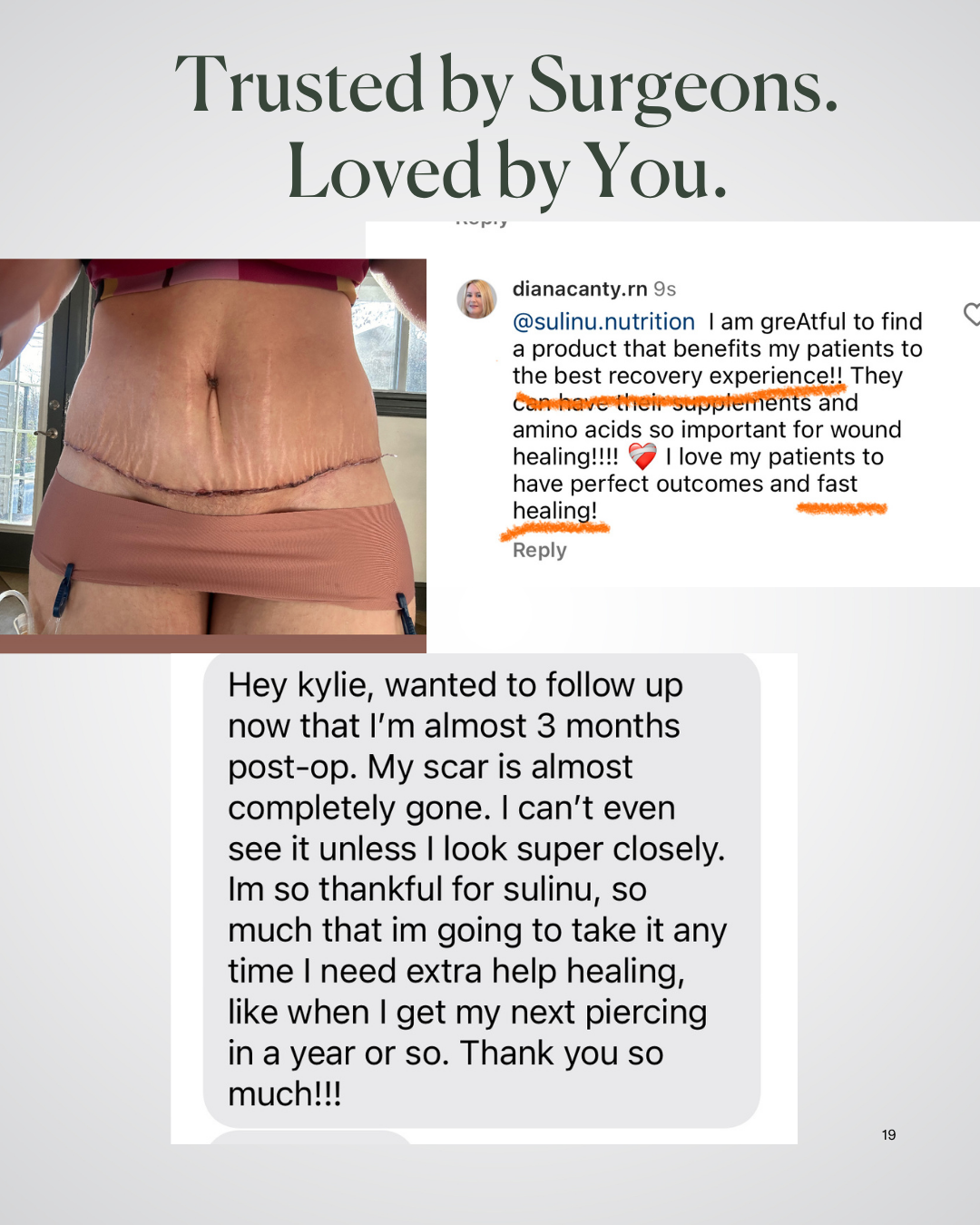
"Can you believe it? [My incision scars] are nearly invisible at just 5 weeks!" -Jessie
Our pre and post surgery supplements are packed with vitamins for wound healing after surgery
- 3rd party tested
- Gluten-Free
- Vegetarian Whey
-
27 Surgeon-Approved Ingredients
- In bioavailable forms
-
5 Patented Ingredients
- Patented is the HIGHEST standard of ingredients
- Faster Incision healing
- Gut microbiome studied
- Clinically tested
- Sourced from Europe and Internationally
- Therapeutic Dosages
Perfect for:
- Before Cosmetic Surgery
- After Cosmetic Surgery
- Slow-to-heal incisions or wounds
- Using a GLP and needing extra nutrition
- Can begin taking at anytime on your surgery journey, EVEN if you are weeks after your surgery! Your scar is healing for a least a year after your surgery date.
How to use:
- Use 1/2 to 1 scoop a day. Max 1 scoop a day for at least 6 weeks postop.
- We recommend 3 bags: Use 1 bag before surgery and 2 bags after surgery
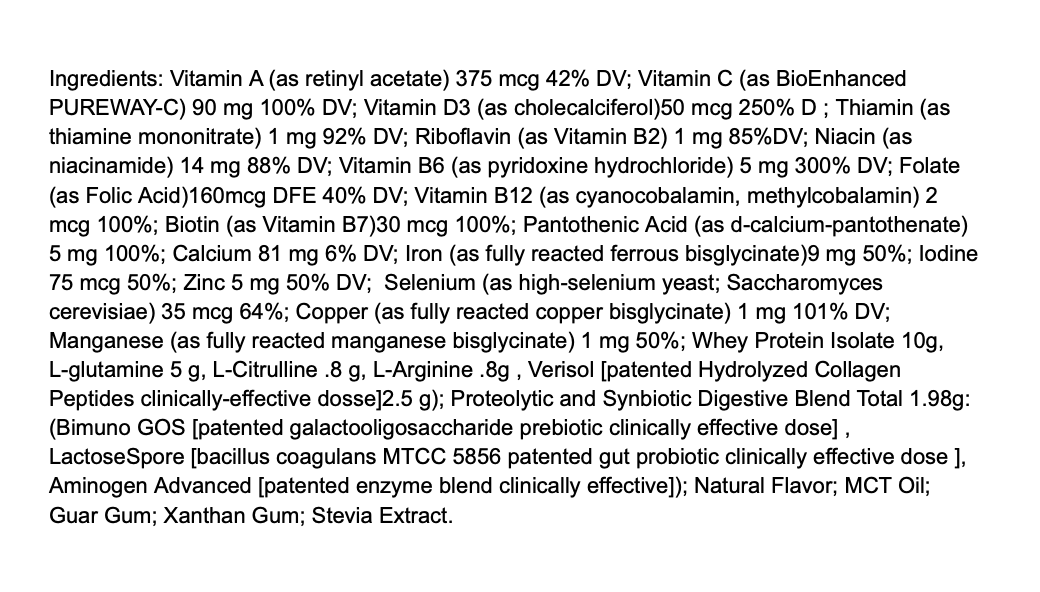
Nutrisurgical Vitamin Powder with Patented, Clinically-tested Ingredients.
All your Protein, Collagen, Amino Acids, MicroNutrients, Synbiotics and Enzymes in ONE SCOOP to give you a seamless recovery after cosmetic surgery.
Note: This product is also commonly used by GLP (Ozempic, Semiglutide, etc) patients to prevent nutrient depletion and Ozempic face
Our Survey Results*:
79% reported a beautiful incision
85% reported a faster recovery
90% liked the taste
X Gluten X Soy X Artificial Colors or Flavors X GMOs
*based upon our postop survey 2024
Introducing BEFORE + AFTER VITALS, the ultimate surgeon-endorsed nutritional supplement tailored exclusively for plastic surgery recovery.
Fears of infection, inflammation, slow-to-heal incisions, and bruising are taken head-on by this super fine, quick-to-dissolve powdered supplement. Add a delicious hit of vanilla flavor to your cold or warm drinks, smoothies, or culinary creations.
1 pouch is 20 servings.
ALLERGY info: Contains lactose. Product was processed in a facility that may also process eggs, peanuts, sesame, soy, tree nuts, shellfish, and other allergens.


